Fungi on the skin are the most common dermatological disease. But the defeat in the legs is considered the most common. Mycoses of the legs and onychomycosis are often found in those who visit public places, in particular hospitals, saunas, baths, swimming pools and gyms.
Each type of fungus has its own characteristics, signs, and treatment methods that anyone who is at risk of getting a fungal infection should be aware of.
What is foot mycosis?
Mycosis, or ringworm, is a dermatological disease caused by a fungal pathogen. The fungus of the skin of the legs is the most common type of this disease, since it is on the legs that the skin is most sensitive, which, moreover, is constantly exposed to the external environment affected by fungus.
Risk factor's
Athlete's foot is common in men who prefer fully closed shoes. Feet begin to sweat and a breeding environment develops. Therefore, most men who have served in the military know firsthand what a skin fungus is. In children, fungal infections occur due to non-compliance with hygiene rules, walking barefoot on contaminated soil, and non-compliance with sanitary rules in kindergartens.

Often, fungal infections of the feet are also found in women with hormonal disorders or decreased immunity during pregnancy. Infection can also occur during a pedicure through non-sterile instruments or towels.
There are common factors that provoke the development of the disease:
- Wearing too tight shoes made of synthetic materials.
- Wash feet infrequently, wear dirty socks.
- Using someone else's shoes, using someone else's towels and other hygiene items.
- Diseases that disrupt blood circulation in the lower extremities.
- Immune system disorders.
- Failure to comply with hygiene standards in public places.
- The presence of calluses, wounds and cracks on the feet.
- Long-term treatment with antibiotics or corticosteroids.
psychosomatics
The causes of the fungus can also be in the emotional state of a person. The medical direction that studies the psychological state of a person and its influence on the development of bodily, psychosomatic diseases, explains fungal infections by the suppression of negative emotions retained inside.
Constant feelings of resentment, anger, feelings of betrayal, or frustration can trigger the fungus or prevent a person from fully recovering.
As a result of these conditions, human immunity is reduced, pathogens present in the body are activated. People with a chronic fungal infection that does not go away with drug treatment should reconsider their internal state or consult a psychologist.
According to many scientists who have studied the psychosomatic causes of the fungus, if you do not work on your character and get rid of negative emotions, the disease will return again and again.
pathogens
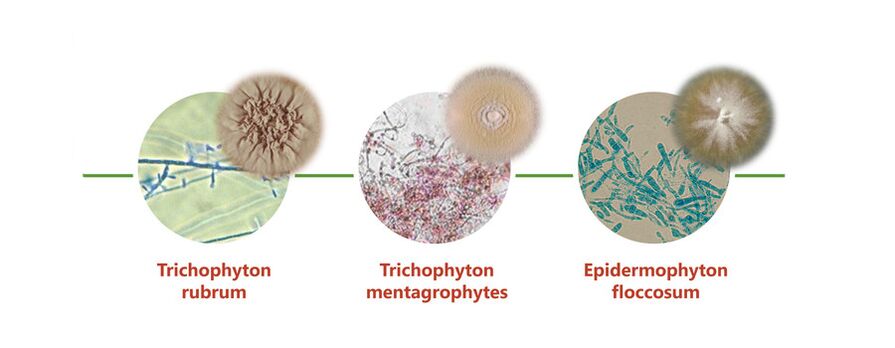
There are a large number of pathogenic microorganisms that can cause lesions on human skin, but the following types of fungi are most often located on the legs:
- Trichophyton rubrum or Tripchophyton purpureum- cause rubromycosis, a disease that most often affects the skin of the feet and nails, but can also spread to other parts of the body.
- Trichophyton interdigitale or Trichophyton mentagrophytes (Trichophytons)- cause epidermophytosis, which develops between the toes, but can also spread to the entire foot area.
- candida- Candida rarely occurs on the feet, but can also affect the interdigital space, the nails and the sole of the foot. It develops predominantly in women.
Mycosis is an infection, and infection can occur in two ways: directly, directly from an infected person to another person, and indirectly, through the floor, shoes, clothing, and other household items with which the infected person has come into contact. It is very easy to get infected with a fungus of the lower extremities: a second contact with any surface or object touched by a person with a fungal infection is enough.
The mechanism of development of fungal diseases begins from the moment the spores enter the human skin. If conditions are favourable, development, growth and reproduction begins.
Microorganisms begin to secrete enzymes that destroy keratin proteins and, consequently, the stratum corneum of the skin. Therefore, itching and discomfort arise in humans. The infection spreads very quickly, the fungi penetrate into the deeper layers of the skin, infecting the surrounding tissues.
If you do not start treatment, very quickly large areas of skin are affected.
But the infection does not always develop immediately after infection, sometimes the fungi remain on the skin or in the shoes for a long period of time. But as soon as the body's defenses are lowered, or a favorable warm and humid environment develops, fungi begin to develop rapidly.
general symptoms
Ringworm of the lower extremities is a very common infection that requires immediate treatment. But not everyone immediately turns to a specialist for help, since they do not pay attention to the primary symptoms or believe that these are signs of other dermatological diseases.
Common signs of skin infection are:
- Redness and peeling of individual areas.
- The appearance of blisters or cracks.
- Itching and burning sensation.
- Dryness and roughness of the skin.
But depending on the location and the pathogen, the disease has various clinical manifestations. The fungus on the heels begins with reddening of the skin and a burning sensation. Over time, bubbles appear, which, when burst, form very painful sores.
Then cracks and scaling-like growths. With a prolonged course of the disease, an unpleasant odor begins to emanate from the affected area, and the infection passes to other areas of the feet and nails.
Fungus on the knees is rare, but if cracks appear on or below the knee that do not go away for a long time, then you should see a doctor. Usually the fungus in this area begins inconspicuously: it begins with redness, then peeling of the skin intensifies, very rarely bubbles form on the surface of the place, which eventually become covered with crusts.
Nail damage, onychomycosis, begins with infection of the skin of the feet. In this case, itching and cracks on the skin may appear, but sometimes the fungus does not touch the skin and affects only the surface of the nail.
Stages:
- normotrophic- at this stage, only the color of the nail begins to change, it becomes yellow, sometimes with a brown tint.
- hypertrophic- the healthy shine of the nail disappears, it acquires an irregular shape, thickens and begins to partially collapse. A person may feel pain when wearing tight shoes.
- onycholytic- the diseased nail is a plate with layers that crumble, thin out, acquire a brownish color. At this stage, the detachment of the nail bed begins.
Manifestations of different types of pathology.
Candidiasis of the legs affects only the soft areas of the skin and nails, without affecting the feet, it can be of two types:
- vesicular-pustular- at the first stage, reddening of the skin with pronounced edema appears. In the future, the affected area is covered with fluid-filled bubbles or purulent mass, in the process they burst and form erosion. Gradually, the inflammatory process subsides and peeling of the foci increases.
- hyperkeratotic- it is rare, it is characterized by a thickening of the stratum corneum with the formation of burgundy scaly furrows.
In most cases, the fungus between the toes is epidermotrophy. The changes in the skin in this pathology can have.jpg) the following forms:
the following forms:
- scaly- between the third and fourth toes, the skin becomes red and sometimes itchy. Very often this stage is overlooked.
- intertriginous- It develops from the first stage. Edema develops, cracks form, and the lesion spreads to neighboring areas. Growths form around the diseased area, making it difficult to wear shoes.
- Sharp- Large accumulations of liquid-filled bubbles form. Wounds and cracks begin to hurt, the general state of health worsens, the temperature may rise.
When the condition is neglected, interdigital pathology covers the nails and the entire area of the sole of the foot, that is, epidermotrophy of the feet develops. The external symptoms are similar to exudative eczema, which complicates the diagnosis.
Rubromycosis of the feet is a simultaneous lesion of the interdigital folds. The skin becomes drier, reddens, severe peeling begins. If treatment is not started in a timely manner, the process passes to the sole of the foot, the lateral area of \u200b\u200bthe feet and the surface of the fingers.
Rubromycosis can also affect other areas of the legs: shins, thighs, buttocks, as well as any part of the body and the head. The lesions are pink spots covered with scaly skin, blisters, or a crust. They quickly grow in size, merging with each other. Rubromycosis of smooth skin usually presents acutely and is accompanied by intense itching.
"I made cracks on my foot, but I did not pay attention. The fungus was discovered during a medical examination at work. The doctor immediately prescribed ointments and pills, also scolded her because it was not applied immediately. "
The details of the traditional treatment.
Fungus therapy on the legs is based on the application of external antifungal agents on the lesions. There are many drugs in the form of ointments, creams, sprays, solutions. Their action is aimed at suppressing the vital activity and reproduction of fungi, as well as slowing down the process of their spread.
Recently, various sprays from the fungus have appeared, which are very convenient to use for external use in the treatment of skin and nail fungus.
During therapy, you can process shoes and clothes so as not to cause reinfection. Disinfectant sprays are suitable for this. Treatment can also be done with antiseptics.
You can use antifungal agents in the form of solutions.
Before applying ointments, you can use a regular solution of salicylic alcohol. It actively acts on fungi, while relieving inflammation and drying suppurating skin areas.
In case of nail damage, it is recommended to use special antifungal varnishes.
There are many different external remedies and they can all be bought at the pharmacy without a prescription. But for the treatment to be effective, it is necessary to know how to use external agents correctly:
- Follow the instructions for how often to apply the medication.
- Hard areas should be steamed before applying the external agent.
- With large dry growths, you can take a bath with soda.
- Treat only the affected areas, without affecting healthy skin.
- After treatment, wash your hands well, without touching other parts of the body, so as not to spread the infection.
In advanced cases, you need to take tablets from the fungus at the same time as using external agents.You can not take pills inside without the recommendation of a doctor; only a specialist can prescribe drugs, depending on the type of pathogen and the severity of the course of the disease.
Treatment of a fungal lesion on the legs at an early stage will not take much time, provided that the drugs are used correctly and the instructions are followed. In severe cases, long-term treatment, up to 3 to 6 months, may be necessary. If the prescribed drugs do not give the desired effect, you should contact a specialist and get new recommendations.
"The fungus on the lower extremities was treated with different ointments for my husband, I tried 8 different pieces, but only tablets from the group of triazole derivatives helped. Well, externally he continued to smear allylamine cream.
Folk methods of treatment
Very often, unconventional methods are used to treat nail and leg fungus.But patients should remember that such remedies are effective at the initial stage of the fungus, and in severe cases they are not always able to help, but, on the contrary, aggravate the course of the disease.
Before getting rid of foot fungus with folk remedies, you should visit a doctor to establish an accurate diagnosis, since the symptoms can indicate various dermatological diseases.

Herbs from the fungus are used to prepare baths, rubs and lotions:
- Pour a handful of calendula flowers with 50 ml of alcohol and 100 ml of water and leave for a day in a dark place. Use it to rub twice a day. Best for nail infections and skin yeast infections.
- Mix dry mint leaves and fine salt in equal proportions. Apply to affected areas for one day, securing with a bandage. Once the time has elapsed, remove the bandage, wash your feet, dry them and repeat. Use only on nails and keratinized skin.
- Five tablespoons of dried celandine pour 100 ml of vodka, leave for two weeks. Use it to clean, trying to avoid contact with healthy skin.
- Prepare two tablespoons of thyme in a glass of boiling water, leave it for an hour and use it for lotions.
You can use tar soap from the fungus:
- Grate a bar of soap, add a little water and melt in a bain-marie, add a tablespoon of tar and 2 tablespoons of any oil. Mix well and pour into molds to make a healing soap. Use it to wash your feet.
- Mix a tablespoon of crushed soap with 2 teaspoons of club soda and add a little water to make a thick mixture. Apply to clean feet at night and apply a bandage on top.
- In the initial course of the disease, it is enough to apply soapy foam of soap for washing to the affected areas of the skin and leave for 15-30 minutes.
Effective Garlic For Fungus:
- Apply crushed garlic to the steamed areas and secure with a bandage. Keep overnight.
- Within 3 days, insist on a mixture of garlic juice, water and vodka, taken in equal proportions. Rub 1-2 times a day on the affected areas.
- Pour 2 finely chopped garlic cloves into a glass of vinegar. Infuse in a dark place for 2 weeks in a container with a closed lid. Use for rubs and lotions.
Vinegar can be used for rubbing or dipping. To prepare a bath, you need to take 100 ml of 9% table or apple cider vinegar per 1 liter of water. The duration of the procedure is 15 minutes, after which you need to remove the softened skin and put on clean socks.
"At work, I walk in shoes for days, my feet constantly sweat, and often a foot fungus appears, I immediately start making vinegar baths and treat all my shoes with it. It passes very quickly. "
consequences and predictions
Many believe that the fungus is not harmful, except for cosmetic discomfort. But yeast infections also carry other threats. First of all, there is a danger that the fungus will spread to other areas of the skin.
From the feet, the infection passes to the skin of the hands, face, torso, scalp. This happens if you do not wash your hands after touching the affected areas of the skin or if the patient's immunity is greatly reduced. From an infected person, infection of family members occurs if sanitation rules are not followed.
With deep injuries, it becomes impossible to wear ordinary shoes, there is severe pain when walking, and when the nails are damaged, the nail bed rises. There is a risk of inflammation of the nerve endings.
Skin lesions, if left untreated, lead to the addition of viral and bacterial infections. The following complications often occur:
- warts
- Phlegmon.
- Pyoderma.
- Erysipelas.
- Malignant mycosis fungoides.
A fungus of the skin of the legs with a prolonged course worsens the functioning of the immune system, patients become more susceptible to allergic manifestations, hives, bronchial asthma, conjunctivitis and rhinitis. Often mycoses are accompanied by atopic dermatitis and eczema. The general condition worsens, weakness occurs, body temperature may periodically rise.
Running fungal infections can lead to internal organ damage.
In addition to physical complications, fungal infections lead to instability of the psycho-emotional state. Infected people become irritable, short-tempered, and often attack others. Nervous system instability slows recovery, so patients may need psychological support.
Toe fungus is very easy to cure if you start therapy at the earliest manifestations of the disease. With daily use of therapeutic agents, the fungus can be eliminated in 10-14 days. But with an advanced infection, the treatment will be longer and more difficult and will not do without the use of systemic drugs. Therefore, doctors recommend not to delay the visit to the clinic.















